by A2 Dental Mallorca | Jul 14, 2025 | Sin categoría
More and more people are interested in enhancing the appearance of their smile. One of the most common questions we hear in clinic is: “Can I have my teeth whitened?” or “Will it make my teeth sensitive?”. But we also hear concerns like “Is it bad for the enamel?” or “Can I use baking soda at home?”.
The truth is that professional teeth whitening is a safe and effective treatment when carried out under dental supervision. However, a number of myths have arisen around this procedure that can lead to confusion or, worse still, to the use of unsuitable or unsafe methods.
At A2 Dental Mallorca, we explain what you should – and shouldn’t – expect from a whitening treatment, and how it can be part of a broader smile design plan.
What is teeth whitening?
Teeth whitening is a cosmetic treatment that lightens the colour of the teeth by several shades using a whitening agent (typically hydrogen peroxide or carbamide peroxide) in a controlled environment.
It can be performed in the clinic with cold light lamps, or at home using custom-made trays. What’s important is that it is always prescribed and supervised by a dentist after a full check-up, since not all patients need the same treatment, and not all stains respond equally.
Teeth Whitening: Facts and Myths
“Whitening damages the enamel” → FALSE
When carried out professionally, whitening does not damage the enamel. Safe concentrations and tested materials are used. What can harm your teeth is using home remedies or non-approved products.
“My teeth will be movie-star white” → IT DEPENDS
Every person has a natural base colour. Whitening can brighten teeth by several shades, but the final result also depends on genetics, habits, and whether the stains are extrinsic or intrinsic.
“I can use lemon or bicarbonate instead” → FALSE AND RISKY
These substances can erode enamel and increase sensitivity. They are ineffective and potentially harmful.
“Whitening is painful” → FALSE
Most whitening treatments are painless or cause only mild temporary sensitivity, which disappears within hours or days. Desensitising gels can also be applied before or after the session.
When is whitening recommended, and when is it not?
Whitening is ideal for healthy teeth that are stained or darkened by coffee, wine, tobacco or ageing. However, it won’t work on fillings, crowns, veneers or intrinsic discolouration from antibiotics like tetracycline.
That’s why a professional evaluation is key. In some cases, your dentist may recommend dental veneers or other aesthetic treatments to achieve a more balanced and long-lasting result.
Whitening and smile design: how are they connected?
Teeth whitening is often the first step in a smile makeover. Many patients want to improve not just the colour, but also the shape, size or alignment of their teeth. That’s why we often combine whitening with:
- Veneers: ultra-thin porcelain or composite shells that cover the visible surface of the teeth to correct imperfections in colour, shape or size.
- Aesthetic contouring: small adjustments to the edges of teeth to enhance harmony.
- Orthodontics: prior treatment in cases of crowding or misalignment that could affect the outcome.
Every smile is different, and based on your needs, we will design a personalised plan that may include whitening, veneers or other minimally invasive procedures.
How long does teeth whitening last?
The effects of a well-executed whitening treatment can last between one and three years, depending on post-treatment care. We recommend:
- Avoiding staining foods or drinks (coffee, wine, tea) and tobacco in the days after treatment.
- Maintaining proper oral hygiene.
- Attending regular hygiene appointments.
- In some cases, a yearly top-up with home trays can help maintain results.
A whiter, brighter smile is within reach
In short: teeth whitening is not harmful when properly done, it’s not a miracle but it is highly effective, and it can help you regain the natural brightness of your smile without compromising dental health.
If you’re thinking about improving your smile, come and speak to us. We’ll examine your gums, your enamel, the nature of any stains and whether whitening or veneers would give you the best outcome.
Because having a whiter smile is not just a matter of looks—it’s also about confidence, ease, and feeling free in your everyday life.
by A2 Dental Mallorca | Jul 7, 2025 | Sin categoría
Do you feel pain in your jaw when you wake up? Do you suspect that you clench or grind your teeth during sleep? Has someone told you that you make noises with your mouth at night, or have you noticed your teeth are becoming worn down? If so, you may be suffering from bruxism—a condition that affects far more people than it seems and can have serious consequences if not treated in time.
At A2 Dental Mallorca, we regularly see patients who come in with headaches, jaw discomfort or tooth sensitivity, unaware that the root of the problem lies in the unconscious habit of clenching or grinding their teeth. Below, we explain what bruxism is, why it happens, how it presents, and what options are available to manage it and protect your oral health.
What is bruxism and why does it happen?
Bruxism is the involuntary activity of the jaw muscles that leads us to clench or grind our teeth repeatedly, usually while sleeping, though it can also occur during the day in moments of stress or intense concentration.
There is not always a single cause, but the condition is commonly associated with emotional stress, anxiety, sleep disorders, certain medications, bite misalignments, or even lifestyle factors.
In many cases, the patient is unaware of what’s happening until the first symptoms appear, or until their dentist detects tooth wear, fractures or signs of overuse in the temporomandibular joint (TMJ).
Consequences of bruxism for your health
Bruxism is more than just an unconscious habit: it can progressively damage both your oral and general health. If not addressed, it may lead to:
- Tooth wear: enamel erosion, shortening of teeth, or fractures
- Jaw pain: discomfort while chewing or opening the mouth
- Headaches and migraines: often upon waking, due to muscle tension
- TMJ problems: joint noises, jaw locking, or clicking sensations
- Tooth sensitivity and gum recession, causing discomfort when eating or drinking
- Disrupted sleep: due to micro-awakenings or interruptions in deep sleep
In more severe or chronic cases, bruxism can also alter the aesthetics of the smile, making the teeth look shorter and aged.
How do I know if I have bruxism?
Bruxism is often diagnosed during a routine dental check-up, when the dentist observes wear patterns on the tooth surfaces, cracks, hypersensitivity, or muscle strain.
Some patients come in after noticing that their partner hears grinding noises at night, others report jaw pain upon waking, or realise their teeth have changed shape. At the slightest suspicion, it is important to get a proper assessment and, if needed, begin treatment early.
Can bruxism be treated? What are the options?
Although bruxism cannot be “cured” in a traditional sense, it can be managed very effectively to prevent dental damage and relieve symptoms. Treatment is always personalised and may include:
- Night guard (occlusal splint): the most common treatment. This is a custom-made device worn during sleep to protect the teeth, redistribute pressure and relax the jaw muscles.
- Complementary therapies: in cases where stress plays a key role, stress management techniques, jaw physiotherapy or psychological support may be recommended.
- Occlusal adjustment and dental rehabilitation: if there are bite issues or advanced wear, restorative dental work may be needed to improve function and prevent further damage.
- Therapeutic Botox (in selected cases): injections into the masseter muscles can reduce the intensity of grinding in patients with severe bruxism.
Treatment should always be guided by a dental professional, as every case is different.
Your sleep and your smile deserve proper care
If you’ve been waking up with jaw pain, notice increased tooth sensitivity or feel tension in your mouth regularly, don’t ignore it. Bruxism is more than just a nervous habit—it can seriously affect your teeth, your rest and your day-to-day wellbeing.
At A2 Dental Mallorca, we carry out a thorough assessment for each patient, identify the source of the problem and offer a personalised treatment plan so you can sleep comfortably again and feel confident that your smile is protected.

by A2 Dental Mallorca | Jul 2, 2025 | Sin categoría
Wisdom tooth pain is one of the most common dental issues among young adults. It usually appears between the ages of 17 and 25, although some people never develop them, or experience no symptoms at all. However, when wisdom teeth do cause pain, it’s important to pay attention: they could be creating complications that go beyond a passing discomfort.
At A2 Dental Mallorca, we frequently treat patients who come to us with pain at the back of the mouth, swelling, difficulty fully opening their jaw, or even fever. All of these symptoms may be linked to the eruption or poor positioning of the wisdom teeth. Below, we explain why this happens, how it presents, and what options exist to relieve the pain and resolve the problem effectively.
Why do wisdom teeth hurt?
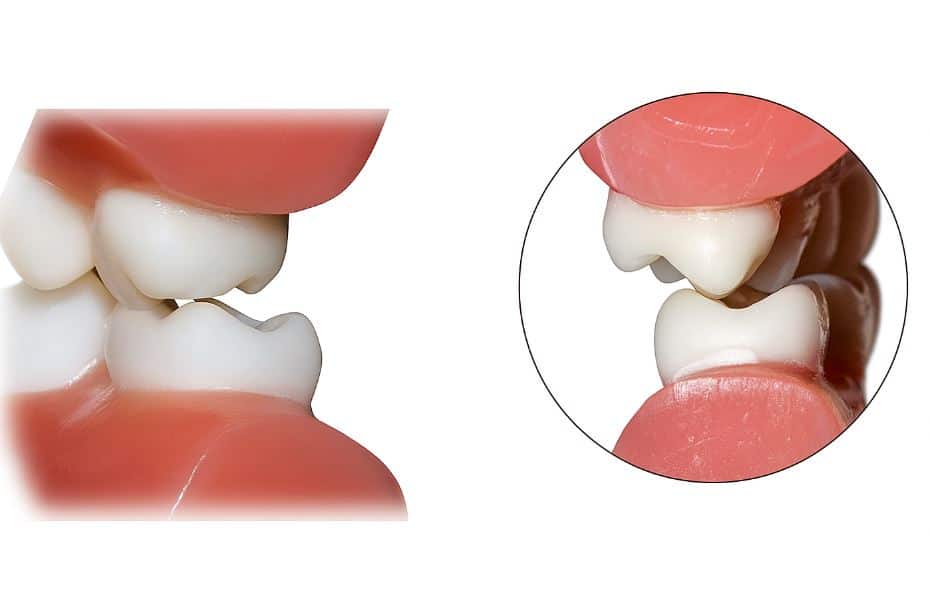
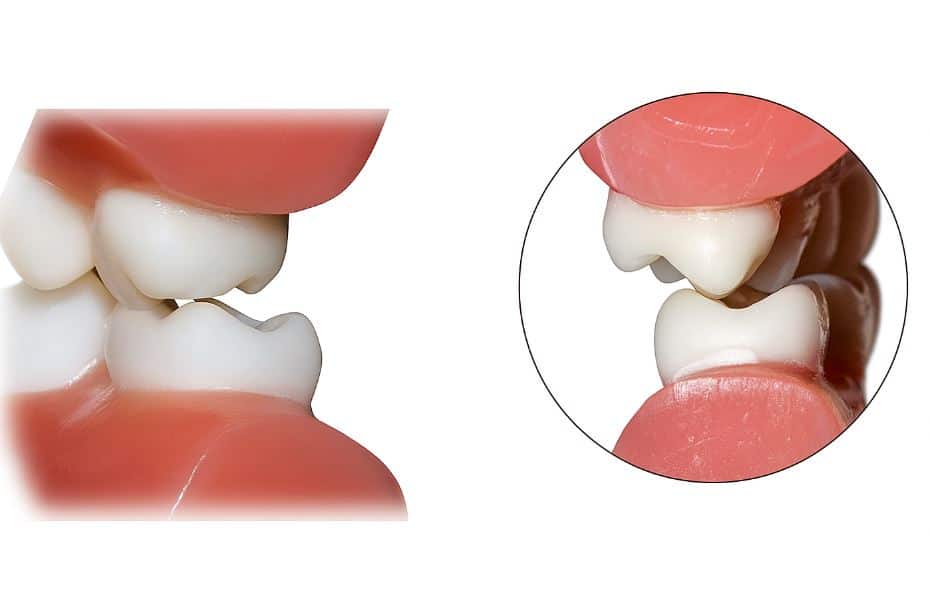
Wisdom teeth, also known as third molars, are the last to come through and often lack the space to erupt properly. This lack of space can cause them to remain partially covered by gum tissue or grow in at an incorrect angle, pressing on nearby teeth or causing inflammation.
Moreover, because they are so far back in the mouth, it’s harder to clean them properly, which encourages the build-up of bacteria. This can lead to infections in the surrounding gum (pericoronitis), decay in the wisdom tooth or the adjacent molar, and even cysts or damage to the roots of nearby teeth.
Typical symptoms when wisdom teeth cause problems
When there is a complicated eruption or an associated infection, the most common symptoms include pain in the back of the jaw, visible swelling, redness of the gum, and sometimes difficulty chewing or fully opening the mouth. It’s also common to notice a bad taste in that area or halitosis if there is an active infection.
In more advanced cases, the pain may radiate to the ear, neck or even cause fever and general discomfort. If it reaches this point, it is essential to see a dentist as soon as possible to prevent the infection from worsening.
When should a wisdom tooth be extracted?
Not all wisdom teeth need to be removed, but those that cause recurrent pain, frequent infections, dental crowding, hard-to-reach decay, or damage to surrounding teeth usually do. In many cases, preventive removal is recommended before more serious problems develop—especially if X-rays show that the tooth has no space to erupt correctly.
At A2 Dental Mallorca, we carry out a full examination using panoramic X-rays or a dental CT scan to determine whether one or more wisdom teeth need to be extracted, and if so, to plan a safe surgery with the fastest possible recovery.
How is wisdom tooth pain treated?
Treatment depends on the cause and condition of the tooth. Sometimes, mild discomfort can be managed with anti-inflammatory medication and good oral hygiene until the eruption completes. However, when there is infection, severe inflammation or difficulty opening the mouth, antibiotics may be required, and extraction may need to be considered.
Temporary relief through warm salt water rinses or applying cold compresses can help, but should never replace a visit to the dentist. Self-medicating or delaying treatment may worsen the condition and make any future procedure more complex.
What to expect after extraction
Many people fear the surgery due to the idea of pain, but it is now a safe and well-controlled procedure. It is performed under local anaesthetic and, if desired, with conscious sedation. The recovery typically involves mild swelling during the first few days, which is easily managed with medication and basic home care.
In most cases, patients can return to their routine within 48–72 hours, following the dentist’s instructions to ensure proper healing.
Personalised assessment and care at A2 Dental Mallorca
If you feel pain at the back of your mouth, have noticed gum swelling, or experience discomfort while chewing, we encourage you not to wait. The sooner your wisdom teeth are assessed, the easier it will be to avoid complications.
At A2 Dental Mallorca, our team will carry out a complete diagnosis and advise you on the most suitable treatment, whether it involves pain management or extraction if necessary. Our goal is to help you regain your oral health with minimal discomfort and maximum safety.

by A2 Dental Mallorca | Jun 30, 2025 | Sin categoría
Keeping your dentures clean and in good condition is not just a matter of hygiene: it is essential for your oral health, daily comfort and self-esteem. However, many people do not know how to care for them properly or whether they are still using the best option for their current situation.
At A2 Dental Mallorca, we explain how to clean your dentures effectively, which mistakes to avoid, and why it is important to visit the dentist to explore whether there are more comfortable or aesthetic alternatives, such as fixed dental implants.
Why is it so important to clean your dentures?
Removable prostheses (whether full or partial) are in direct contact with gums, mucosa, and sometimes with natural teeth. If they are not cleaned properly:
- Food particles, bacterial plaque and fungi such as Candida albicans build up.
- Bad smells, stains, and dry mouth may occur.
- The risk of infections or gum irritation (prosthetic stomatitis) increases.
- The lifespan and fit of the dentures are reduced.
Good hygiene protects your health, prolongs the life of your dentures and improves your daily quality of life.
How should dentures be cleaned? Step by step
1. Remove the dentures after each meal
It is essential to remove the dentures at least twice a day (ideally after each main meal) to remove food debris and prevent fermentation.
2. Wash them with a specific brush
Use a special denture brush (not a regular toothbrush, which may damage them) and lukewarm water—never hot.
Do not use standard toothpaste: it is abrasive and can scratch the surface. Instead, choose neutral soap or products specifically made for dentures.
3. Use effervescent cleaning tablets (optional, do not replace brushing)
These can help eliminate bacteria and odours but are not a substitute for manual cleaning. Ask your dentist if they are suitable in your case.
4. Brush your gums and tongue as well
Even if you have no natural teeth, gently brush your gums, palate and tongue with a soft-bristled brush to remove bacteria and stimulate blood flow.
5. Store the dentures in water or a clean, dry container
When not in use (e.g. overnight), store your dentures in a closed container with clean water or as recommended by your dentist. Never leave them exposed to the air, as they may become misshapen.
Common mistakes when cleaning dentures
- Using regular toothpaste (it can scratch and deteriorate the surface).
- Cleaning with bleach or vinegar (can damage them and irritate soft tissues).
- Brushing them too hard or with hard brushes.
- Storing them without water, which may deform their structure.
- Not brushing the gums or inside of the mouth, where bacteria also build up.
What if the dentures no longer fit properly or move?
Over time, the bone structure of the jaw and maxilla changes. A denture that once fitted well may begin to move, cause discomfort, or interfere with speech and chewing.
If you notice any of the following:
- Your denture no longer fits as it used to
- You develop sores or irritation
- You find it difficult to speak or chew certain foods
- You avoid laughing or speaking for fear it might move
It’s time to visit the dentist to review your options.
Should I keep using removable dentures or are there other alternatives?
Today, there are more comfortable, fixed and aesthetic solutions, such as dental implants, that allow you to regain the function and appearance of your teeth permanently.
Some alternatives worth considering:
- Individual implants (for those missing just a few teeth)
- Fixed prosthesis on implants (such as the All-on-4 or All-on-6 techniques)
- Implant-retained overdentures, which combine stability with the option of removal for cleaning
Why visit your dentist if you wear removable dentures?
A dental check-up allows you to:
- Check if your denture is still functional and safe
- Assess whether there is bone loss or irritation
- Learn about more modern, fixed and aesthetic alternatives
- Improve your confidence, independence and overall quality of life
A well-designed smile, whether with a prosthesis or implants, gives you the freedom to speak, laugh and eat without worry, and is an investment in your long-term well-being.
Haven’t had your dentures checked in a while? Let’s talk
At A2 Dental Mallorca, we offer a full assessment to evaluate the condition of your denture and explore whether there are more up-to-date, functional options for your specific needs.
Book your free consultation and take the first step towards a more comfortable, secure and natural smile.

by A2 Dental Mallorca | Jun 26, 2025 | Sin categoría
Have you ever noticed a persistent metallic taste in your mouth, similar to iron or rust? Although it may seem like a one-off issue, in many cases this symptom can be a sign of an oral health problem or general medical condition that deserves attention.
At A2 Dental Mallorca, we explain why a metallic taste occurs, when you should be concerned, and the role of good oral hygiene and regular dental check-ups in preventing and treating it effectively.
What is a metallic taste in the mouth and why does it happen?
A metallic taste in the mouth, known medically as dysgeusia, is a taste disorder that causes a persistent metallic or bitter taste, even when you haven’t eaten or drunk anything unusual.
It can be temporary (for example, after a deep cleaning or due to medication) or chronic, if it lasts for several days or weeks. In the latter case, it is advisable to consult a specialist.
Most common causes of a metallic taste in the mouth
1. Plaque and tartar build-up
One of the most frequent causes is poor oral hygiene. Bacterial plaque, especially in hard-to-reach areas, can release sulphur compounds that alter the taste in the mouth.
In more advanced cases, if gingivitis or periodontitis is present, this unpleasant taste is also common.
2. Bleeding gums
Inflamed or bleeding gums can leave a slight metallic taste due to the presence of blood. This is a clear sign of gingival inflammation and requires professional attention.
3. Oral infections
Infections such as abscesses, deep cavities or periodontal infections can release compounds that alter taste. They are often accompanied by bad breath or localised pain.
4. Medications
Some medications—such as antibiotics, antihypertensives, or anxiety treatments—can cause dysgeusia as a side effect. If this is the case, you should inform your doctor or dentist.
5. Dry mouth (xerostomia)
A lack of saliva reduces the mouth’s natural cleaning effect, encouraging bacterial growth and unpleasant tastes. This may be related to stress, medications or systemic problems.
6. Nutritional deficiencies or systemic diseases
Deficiencies in vitamins (such as B12), diabetes, hormonal changes, or kidney or liver disorders can also lead to a metallic taste as a secondary symptom.
When should a metallic taste be a concern?
Although it’s often temporary, you should see your dentist if the metallic taste lasts longer than 48–72 hours or appears alongside other symptoms such as:
- Swollen or bleeding gums
- Toothache or sensitivity
- Persistent bad breath
- Dry mouth or burning sensation
- Ulcers or lesions in the mouth
Early diagnosis can prevent more serious complications.
The importance of oral hygiene in prevention
One of the most effective ways to prevent metallic taste related to the mouth is to maintain a strict oral hygiene routine:
- Brush your teeth at least twice a day with fluoride toothpaste
- Use dental floss or interdental brushes daily
- Rinse with a suitable mouthwash, as recommended by your dentist
- Schedule a professional cleaning every 6 months to remove tartar
- Don’t forget to brush your tongue, where many bacteria accumulate
Seeing your dentist: key to a healthy mouth and fresh taste
In many cases, a metallic taste is a sign that something isn’t right with your oral health. Visiting your dentist regularly allows you to:
- Detect and treat oral infections before they worsen
- Monitor gum health and prevent progression of periodontal disease
- Assess for bruxism or faulty restorations that may cause discomfort
- Receive guidance on hormonal, nutritional or medication-related issues that affect your mouth
At A2 Dental Mallorca, we carry out a full assessment to identify the origin of the symptom and apply the most suitable treatment, from a deep clean to medical follow-up if necessary.
Have you noticed a metallic taste in your mouth? Don’t ignore it
A metallic taste could be your body’s way of alerting you to improve your oral care. At A2 Dental Mallorca, we help you regain your oral well-being with preventive and personalised treatments.
Book a free check-up and we’ll answer all your questions with the care and professionalism that define us.